Former Health Minister Aneurin Bevan who spearheaded the founding of the NHS in 1948
View this article on our brand new website: http://politicsbulletin.co.uk/digital-health-the-future/
Since its foundation in 1948, the NHS has been a key characteristic of the United Kingdom. It was created out of the ideal that good healthcare should be free to all, regardless of wealth and hitherto it has been a monumental success with many countries across the world striving to replicate the National Health Service for their own citizens. However, the past few years have seen the NHS hit turbulent times with politicians using it as a political football to kick around at will. The NHS has currently come to a stand still in terms of its future projection – it has fallen behind the health services of various Scandinavian countries and according to research by The Kings Fund, by 2020, Britain’s spending on its health service will be £43 billion less a year than the average spent by its European counterparts such as France and Germany. Britain’s GDP investment into its health system is at an all time low and because of this critics have labeled Britain the “sick person of Europe.”
So why is the NHS in decline? Well firstly it costs the government and indeed the tax payer well over £100 billion to fund the NHS each year – compare this with the cost to run the NHS in 1948 which, after adjusting for inflation was roughly £9 billion at today’s value. As aforementioned, the British government is planning on spending less of its GDP per year on its National Health Service compared to previous years and there is no doubt that less money will mean a lesser service provided. According to some experts, when looking at the NHS in it’s current nature and comparing it with services in Scandinavia, the UK has probable lost 3-5 years already.
Last week the UK Health Secretary Jeremy Hunt initiated plans to fund the NHS with £4 billion in order to “create a paperless NHS”, Hunt wants the NHS to use technology to its advantage and that means investing in Digital Healthcare.
The Present
In basic terms, Digital Health is essentially the use of technology and communication networks to improve the service offered by heath providers for the care of patients and the population. Innovators in the field of digital health are focused on using new technology to improve the healthcare experience for both healthcare staff and patients.
According to one innovator in the field of digital health, Peter Ohnemus, the UK must ‘rectify its strategy on digital health,’ he said: “The UK has lost a lot of time and money as there is not a clear digital health strategy within the NHS. This has to change very rapidly or the NHS will have very serious financial and delivery problems – this cannot be in any UK politicians or citizens interest.”
 Ohnemus, who’s company dacadoo recently won the 2016 BIG Innovation Award 2016 regards investment into digital health for all health care groups and governments across the world as paramount because of the advantages digital healthcare would permit to the tax payers, patients and health care staff: ” Digital healthcare is here today and can save up to 25% of our healthcare spending today. Digital sensors/mobile health at home can save up to 80% of the hospital visit cost. The upfront investment in England is probably 10% of the overall healthcare cost and long term it will provide cost savings of 15-25%.
Ohnemus, who’s company dacadoo recently won the 2016 BIG Innovation Award 2016 regards investment into digital health for all health care groups and governments across the world as paramount because of the advantages digital healthcare would permit to the tax payers, patients and health care staff: ” Digital healthcare is here today and can save up to 25% of our healthcare spending today. Digital sensors/mobile health at home can save up to 80% of the hospital visit cost. The upfront investment in England is probably 10% of the overall healthcare cost and long term it will provide cost savings of 15-25%.
“Digital healthcare means that you can track, document and improve your health in real-time over your smart phone. It means that elderly people can live in their private homes a lot longer and have assisted living at very low cost. People from the ages of 30-65 can have their lives followed and improved on their smartphone. In the future you can track your blood pressure, blood values, health and weight in real-time wherever you are at a very low cost. That is digital health.”
Technological advancements in healthcare have meant that progress has been achieved in all fields of Digital Health thus far, from medical devices used directly by doctors to mobile health and computers that aid in health management and diagnosis. Aakash Ganju, the CEO of Mirai Health – a website and smart phone app dedicated to improving health care outcomes for both patients and doctors, believes that Digital Health has “put a lot more information into the hands of the consumer whilst it has also pushed doctors to becoming substantially more communicative with patients.”
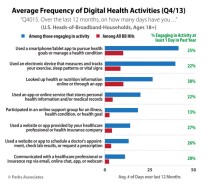
Digital Healthcare activity within the average American household
According to statistics by the Deloitte Centre, UK smartphone use has risen by 8% within the last year alone whilst at least 80% of all health care consumers in the UK have a smart phone and internet access. It is to be expected that this trend will continue to rise and many experts believe that it is imperative health care providers make use of this information and act now. New technology has allowed patients to be able to access their medical records online as well as book appointments with their GP using their mobile phone – and this is only the beginning.
The Future
It is an ever increasing trend that technology is improving industries throughout the world and Jose Miguel Cacho – a professional in Digital Health, finds it curious why governments wouldn’t invest heavily in new technology for healthcare: “By comparison few people doubt the benefits of digital banking or online travel services. Digital health is not only necessary, it’s just that, it’s necessary to bring to the population processes to improve their overall health, which are based on the technology we use today.”
But are the improvements in Digital Healthcare worth the extra costs? Only time will tell. Peter Ohnemus believes that like any new innovation you first have to invest and then you will receive the pay back: “It will provide a lot of jobs and growth going forward, if politicians do not act the jobs will go to other countries – Digital does not know borders.
“In terms of the future for healthcare I personally believe that the brightest minds in digital are today working on digital outcome and digital bio-sensors that will be able to track our life in a ‘passive non-invasive way.’ Meaning that we can calculate your health in real-time and hopefully get the right ‘wrong’ signals early and help people have a healthier and happier life at the end of the day.”

A growing trend in Digital Health funding in the USA
Global companies such as Apple and Google are also investing heavily in Digital Health. Google have created Verily.com a website which researches how ‘technology can be implemented to create a true picture of human health’ whilst Apple are investing heavily in Digital Health mobile apps – apps such as docadoo enables users to track, manage and benchmark their health in an easy and fun way on their smartphones using a variety of techniques from online games to social features – healthcare truly is changing.
However, with huge amounts of capital being poured into Digital Health, innovators should not take their fingers off the button, Aakash Ganju said: “There have been many false starts (IT deployment in the NHS, for example) and missed expectations. We have to keep the bar high and make sure that the stakeholders in driving Digital Healthcare adoption are multidisciplinary and appreciate the unique dynamics of healthcare ecosystems. We can’t afford to celebrate ‘inputs’ and must really focus on measuring the ‘outputs’ of digital interventions. Only then will we know if the improvements are worth the extra costs.”
It seems set that if money is invested into new technology wisely then the world should see a digital healthcare revolution with improved healthcare systems all over the world for patients and staff. Unsurprisingly, innovators and entrepreneurs working within Digital Health are excited to sell the products they have created and patented to health organisations across the globe but it is imperative that patient happiness and healthcare comes before profits; only when we see an improved healthcare system that is backed up by doctor and patient happiness statistics as well as an improved level of health and well – being for patients will we know that government investments into Digital Health have succeeded. The future of healthcare is almost certainly in Digital Health but it needs to be implemented in the correct way – that there is no doubting.





